Ameliyatlar
7:39
12:11
26:40
5:47
9:07
7:47
8:39
10:36
9:40

2:45
2:25
10:45
15:20
5:41
3:51
4:20
7:39
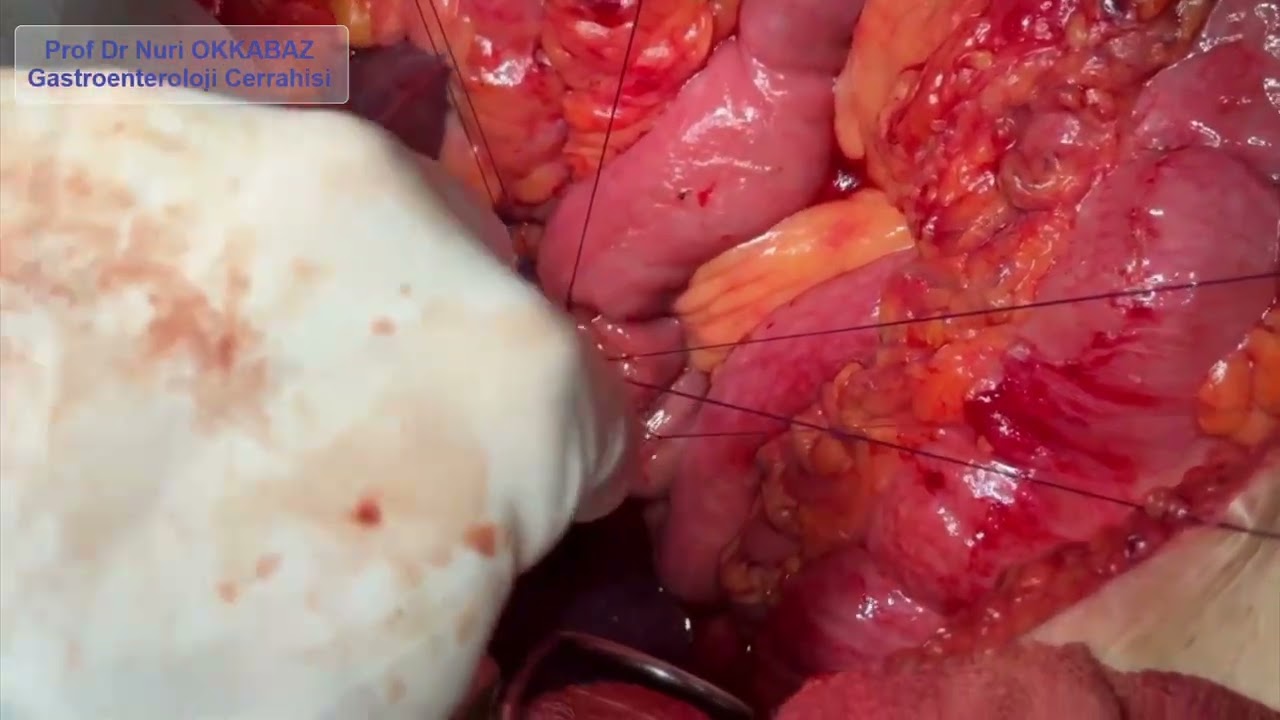
In cases such as bile duct tumors, pancreatic tumors, bile duct cysts, or bile duct strictures or injuries, it may be necessary to connect the bile duct to the small intestine.
There is no special equipment used for this anastomosis between the bile duct and the intestine; it is performed using a hand-sewn technique.
This anastomosis can be carried out with a single surgical suture in a continuous fashion, or—depending on the surgeon’s preference—by placing individual interrupted stitches.
In this video, you can watch the surgical footage of a patient in whom we performed an end-to-side anastomosis between the bile duct and the small intestine using the interrupted suture technique.
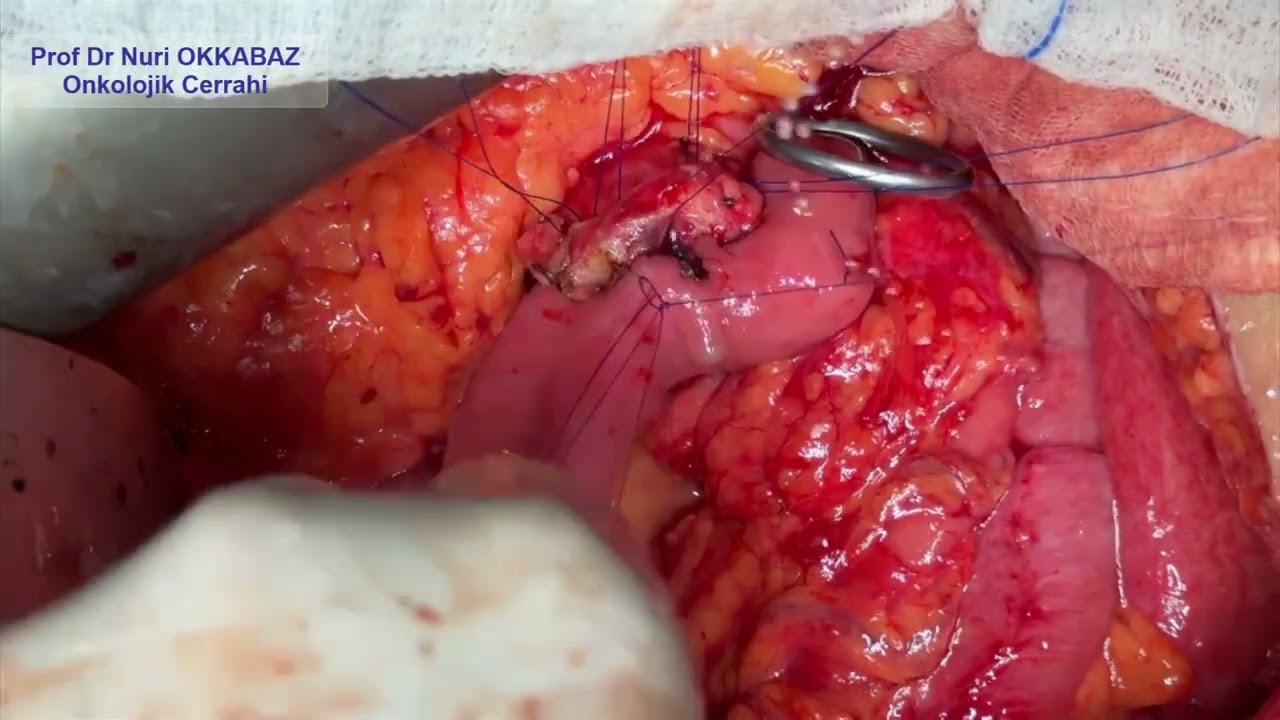
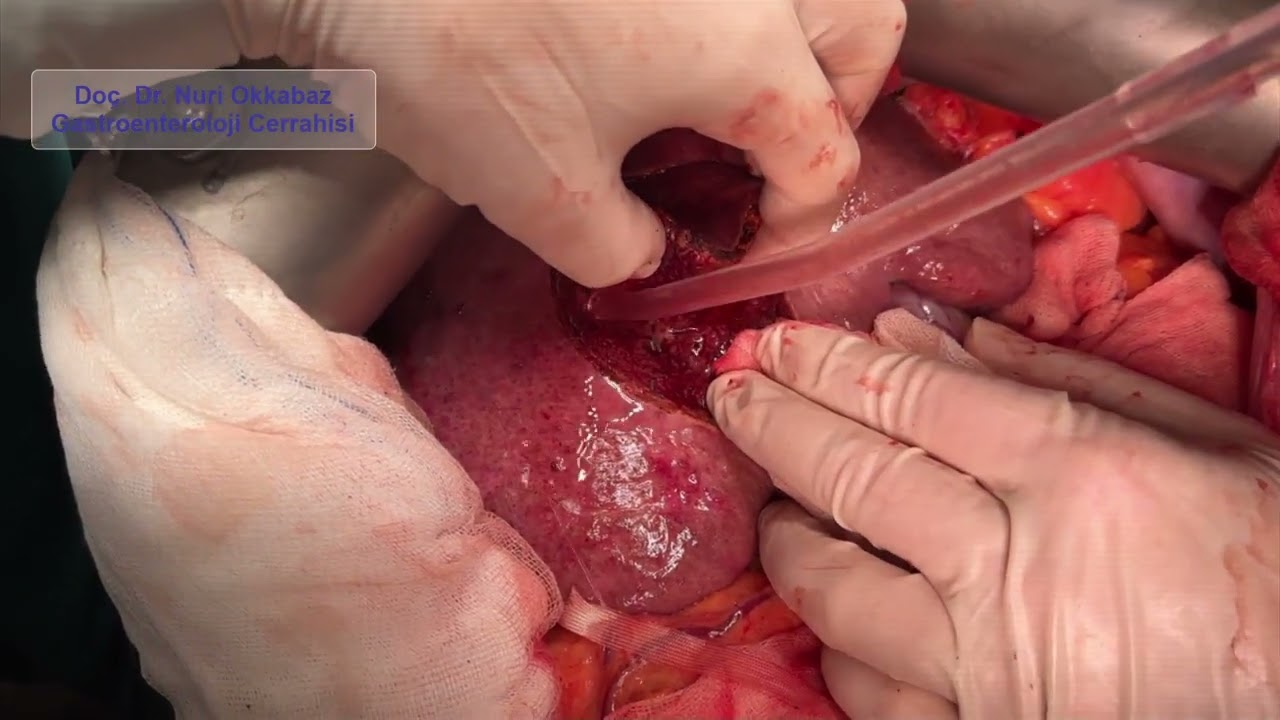
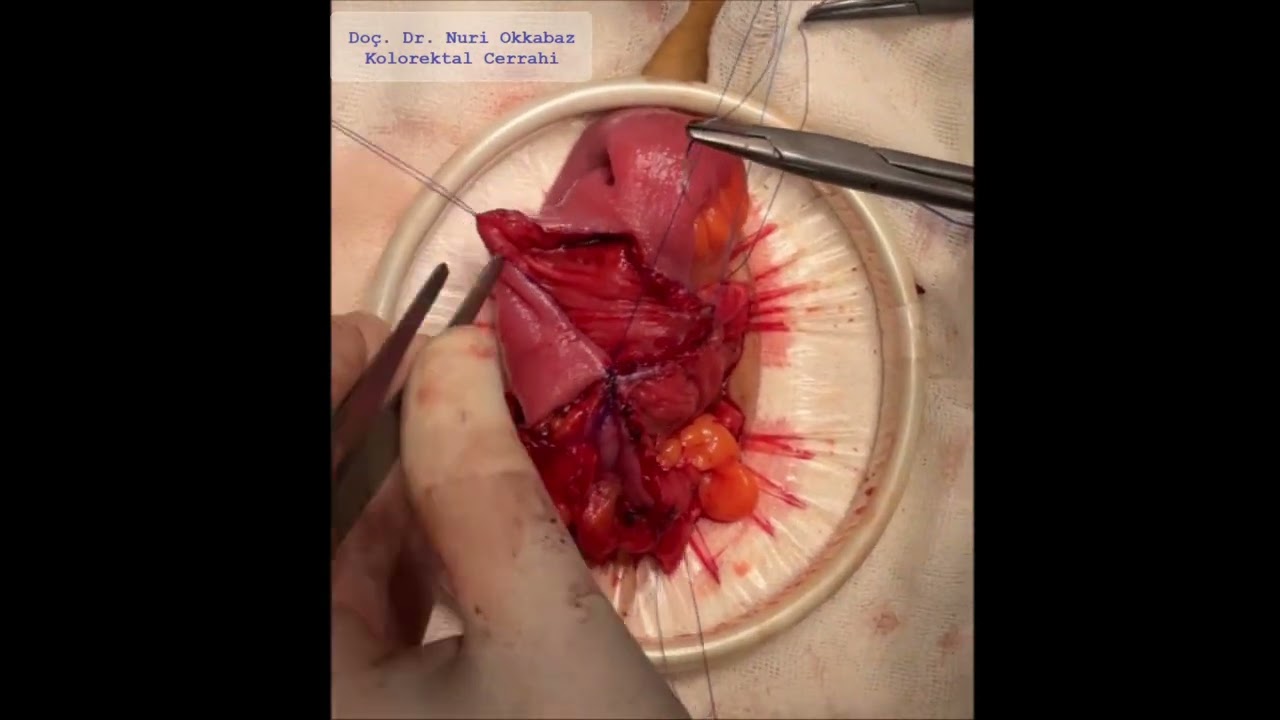
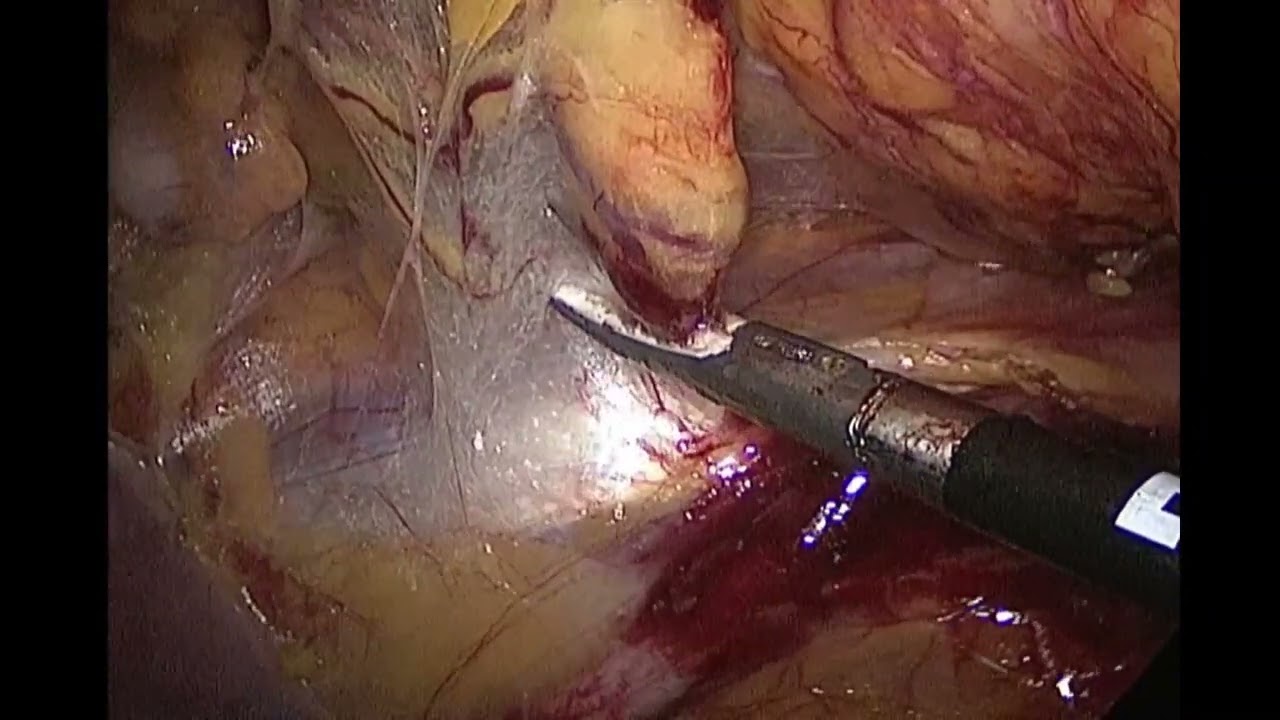
After pancreatic surgery performed for tumors of the pancreas, distal bile duct (choledochus), duodenum, and ampulla of Vater, one of the most important steps of the operation is the connection of the pancreas to the intestine.
If leakage or seepage occurs from this area within the first week after the surgery, it can lead to life-threatening complications. Therefore, the pancreatic anastomosis must be performed with great precision.
Although many anastomosis techniques have been described for this region, the Blumgart-type anastomosis is considered the safest method.
You can watch footage of the Blumgart-type pancreatic anastomosis performed during a recent Whipple procedure I carried out for pancreatic cancer in the video.
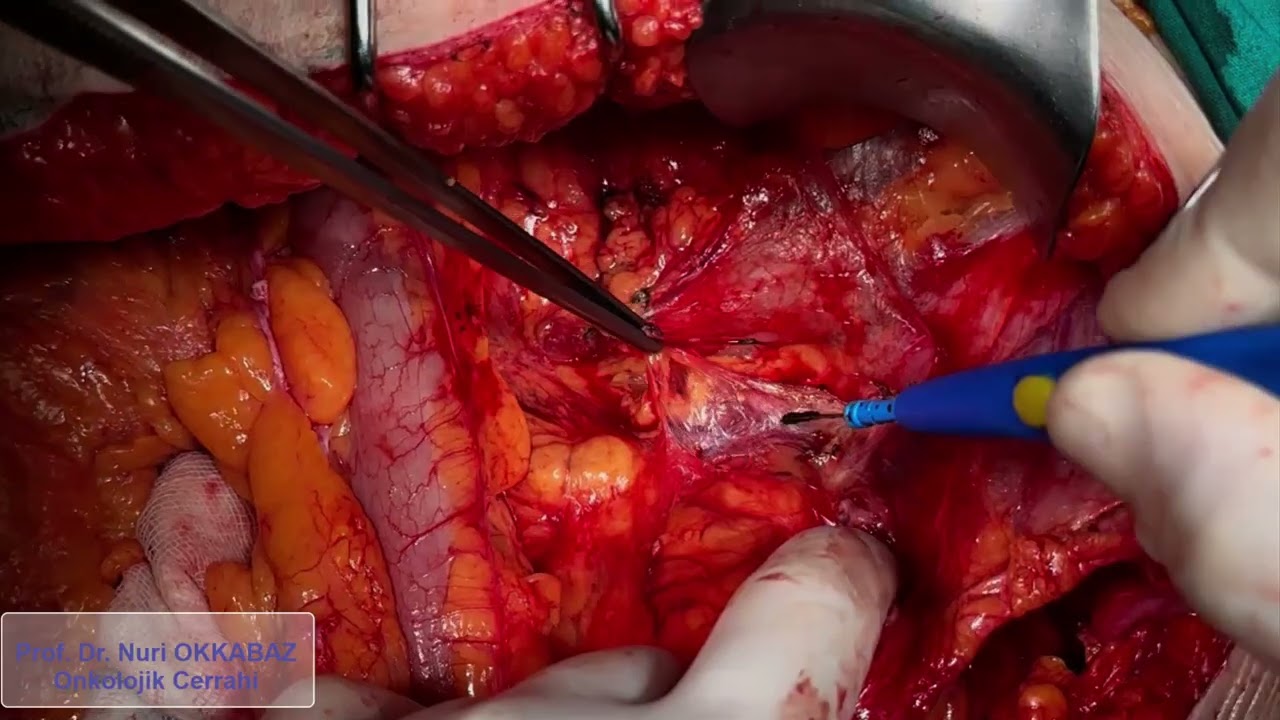
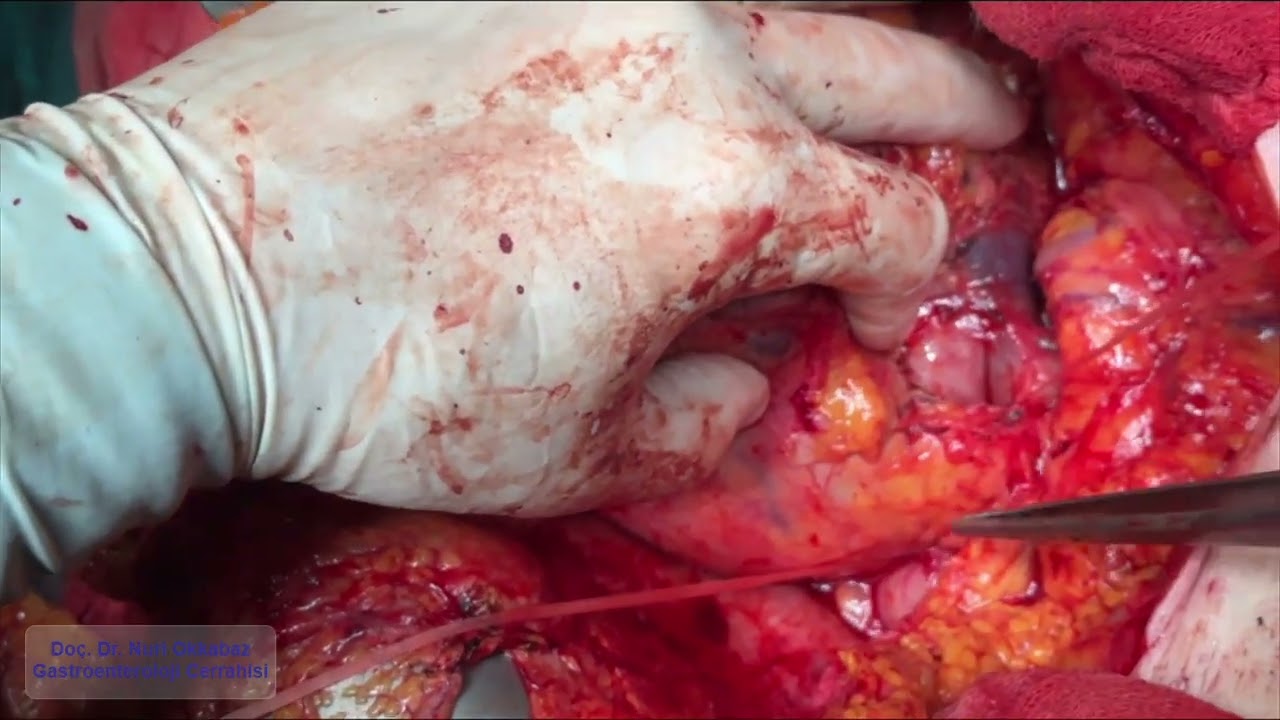
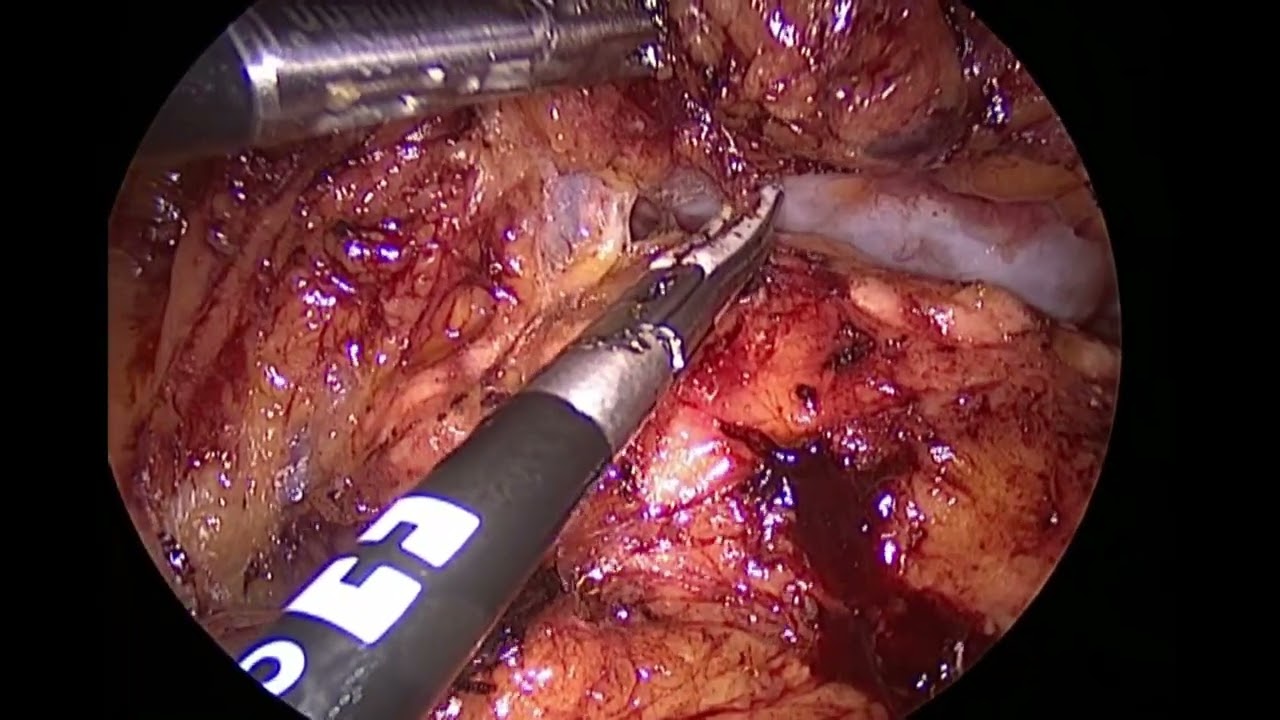
In many types of cancer that have spread to the peritoneum, especially colon cancer, performing an operation called cytoreductive surgery — in which all tumor foci in the abdomen are removed — followed by the application of heated chemotherapy (HIPEC) into the abdominal cavity may provide a chance to be cured of the tumor.
For this method to be applied, certain oncological and surgical criteria must be met. Although we perform the surgery in suitable patients, there are some risks during and after the operation. Therefore, it is very important that this surgery be performed by experienced hands in order to minimize these risks.
Although heated chemotherapy seems to be the most prominent part of these surgeries, the essential point is that the tumor must be completely removed to the extent that it cannot be seen with the naked eye. Heated chemotherapy applied while leaving behind residual tumor tissue will not result in complete elimination of the disease.
I hope that the surgery video of our patient, who developed peritoneal spread due to colon cancer, will be useful for patients and colleagues who wish to learn more about this topic.
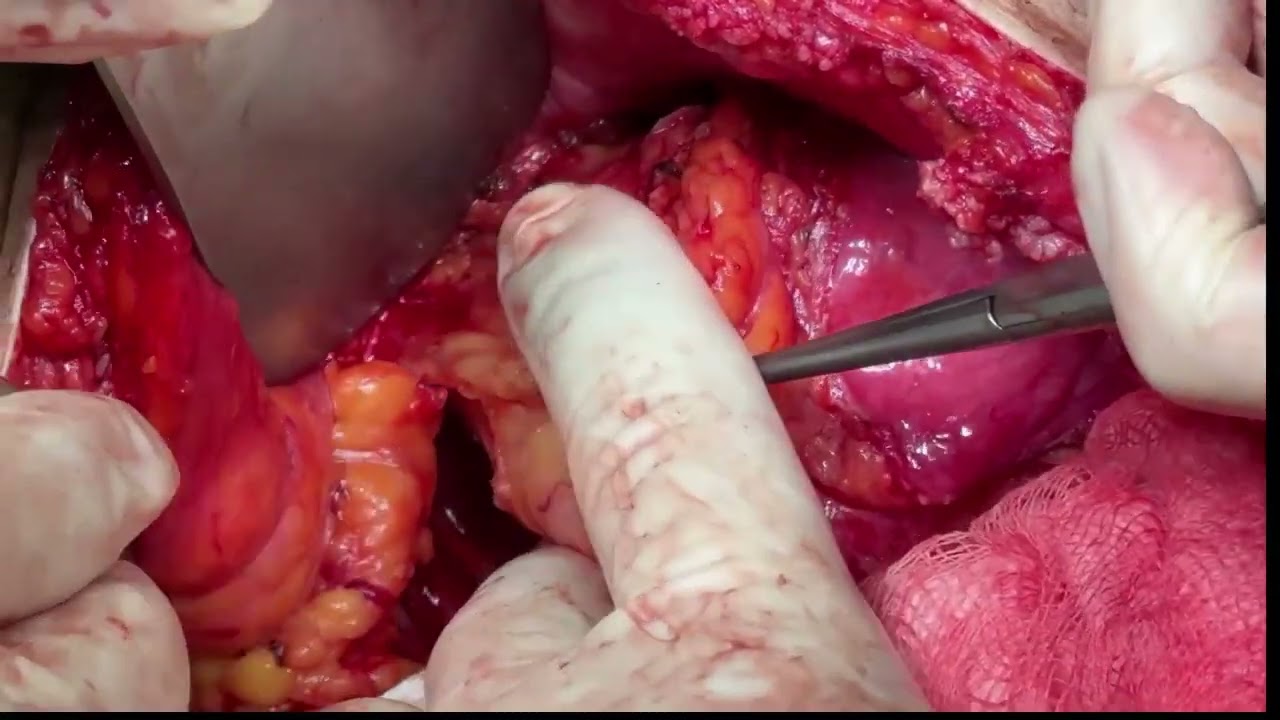
This video shows the surgical removal of a tumor mass that developed at the previous surgical site in a patient who underwent surgery for right colon cancer. The tumor occupied the right retroperitoneal space and was adherent to the abdominal wall.
During the resection of this very firm tumor tissue, the intestines, urinary tract, and kidney were carefully preserved, although part of the abdominal wall muscles had to be removed.
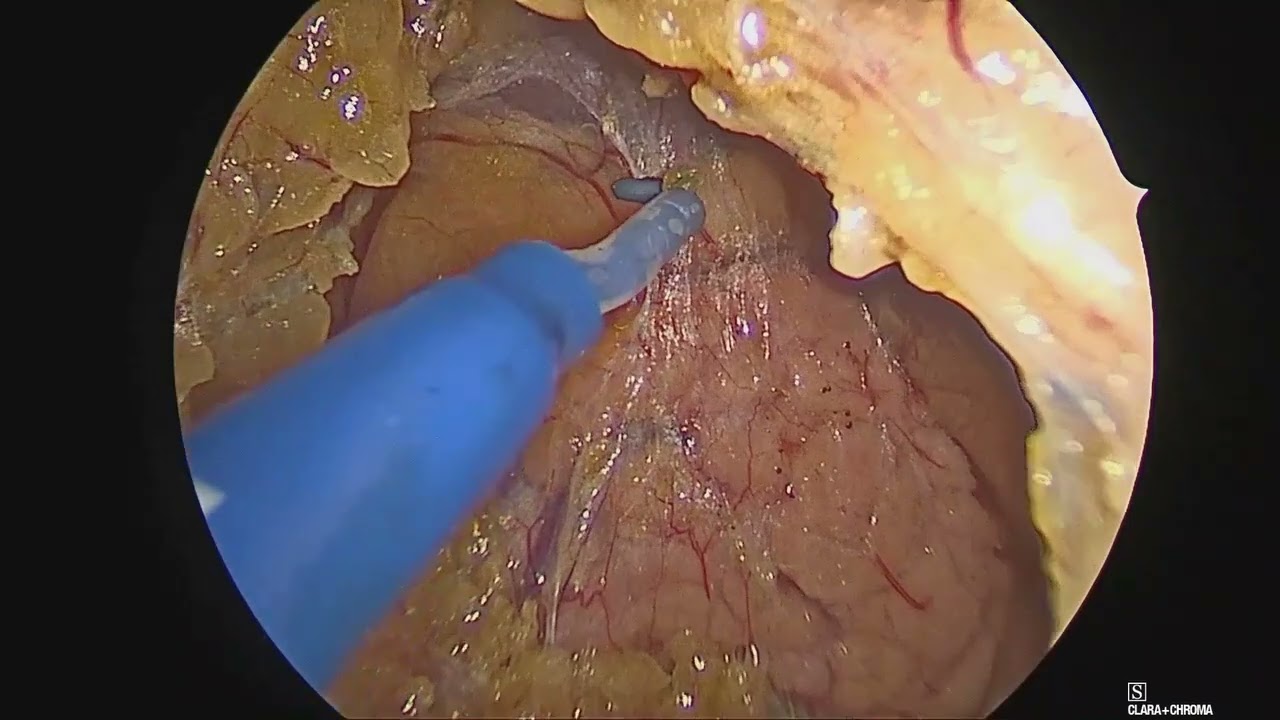
In cases of colon cancer, surgical removal of liver metastases is a viable treatment option when feasible.
This video demonstrates the step-by-step resection of a liver metastasis originating from colon cancer using a conventional surgical technique.
With this approach, metastatic lesions — or any hepatic mass — can be removed with minimal bleeding, significantly reducing surgical risks and enhancing patient safety.
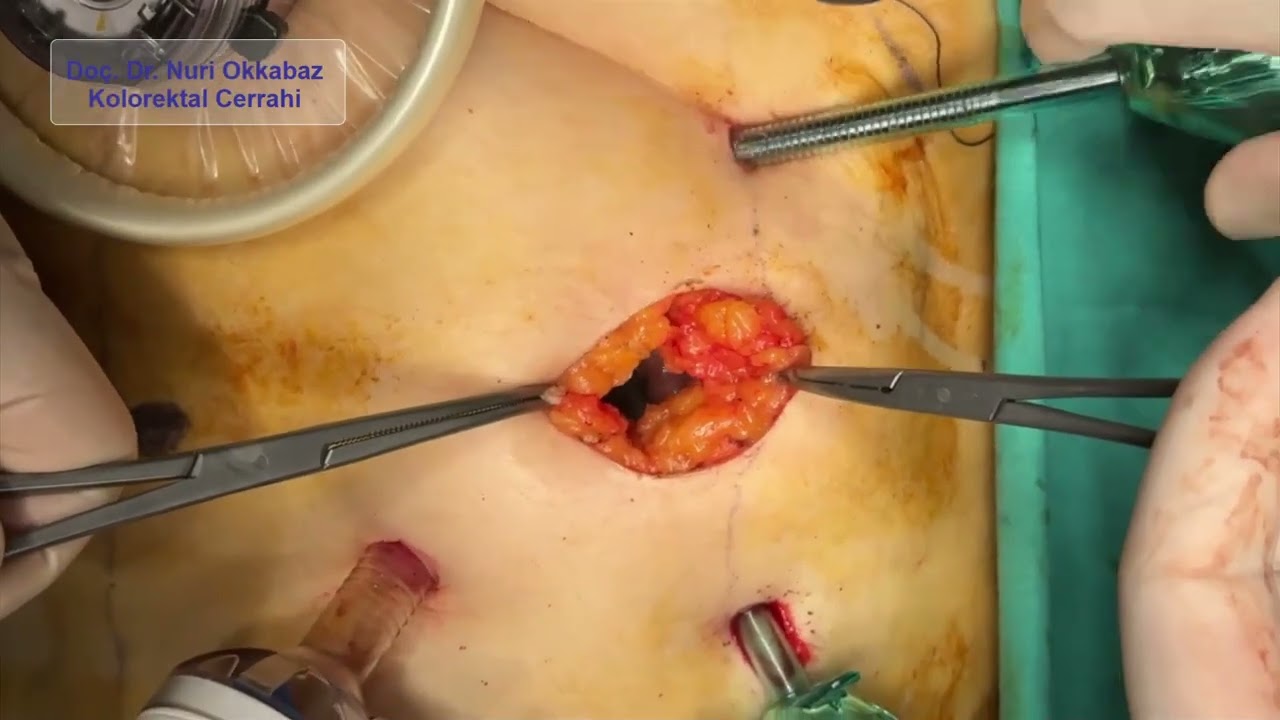
In patients undergoing laparoscopic low anterior resection for rectal cancer, a colorectal anastomosis is created to reconnect the bowel to the anus. To protect the anastomosis and prevent stool from reaching the surgical site during the early healing phase, a temporary diversion of the small bowel to the abdominal wall can be performed.
This procedure is called a loop ileostomy or diverting ileostomy.
In this video, you can observe the step-by-step surgical process of ileostomy creation.
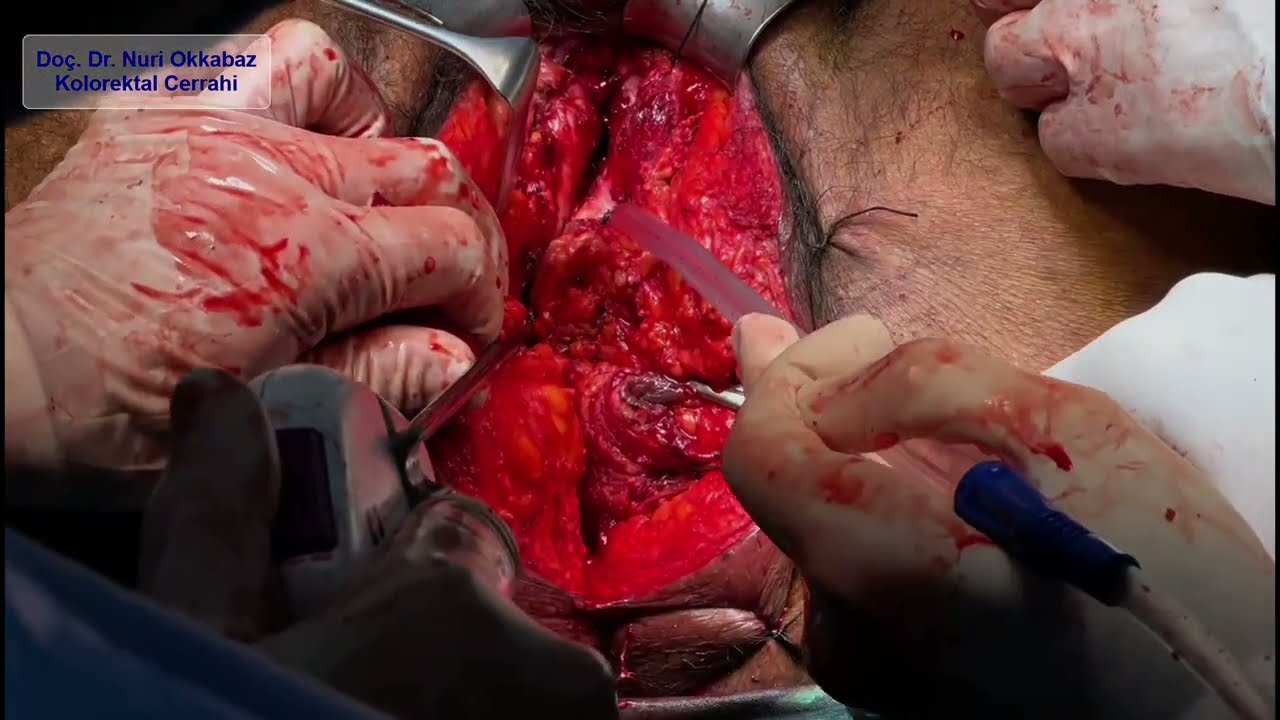
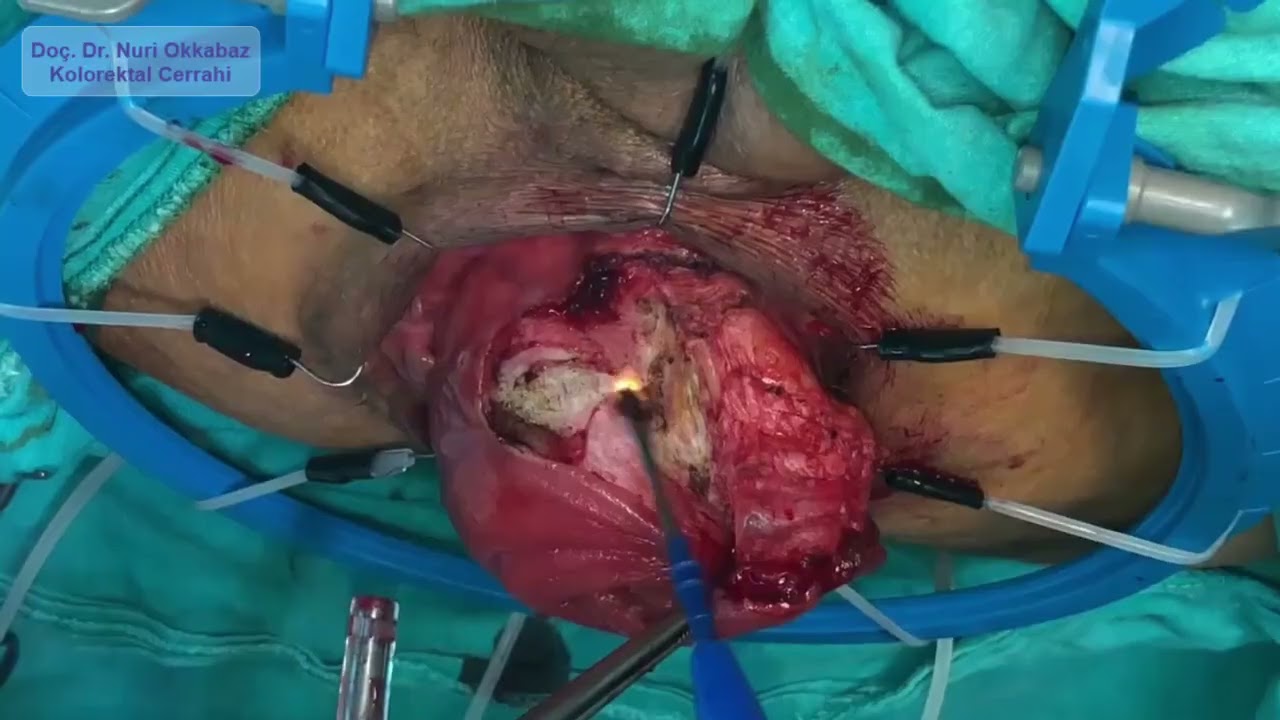
In cancer surgery, the fundamental principle is to remove the involved organ partially or completely, without leaving any residual disease. In pelvic tumors, due to the anatomical proximity of organs, resection may involve not only the primary organ but also adjacent structures. This principle applies to both primary and recurrent tumors — the goal is always complete resection.
Pelvic exenteration may be necessary when rectal, gynecological, or urological cancers invade neighboring organs. In male patients, this procedure typically involves en bloc resection of the rectum, bladder, and prostate; in female patients, it may include removal of the rectum, uterus, vagina, and/or bladder, depending on tumor involvement.
In this video, we present the perineal phase of a pelvic exenteration performed in a patient with locally advanced rectal cancer who had previously undergone radiation and prolonged chemotherapy. At another center, surgery had been attempted but the tumor was deemed unresectable, and a colostomy was created instead.
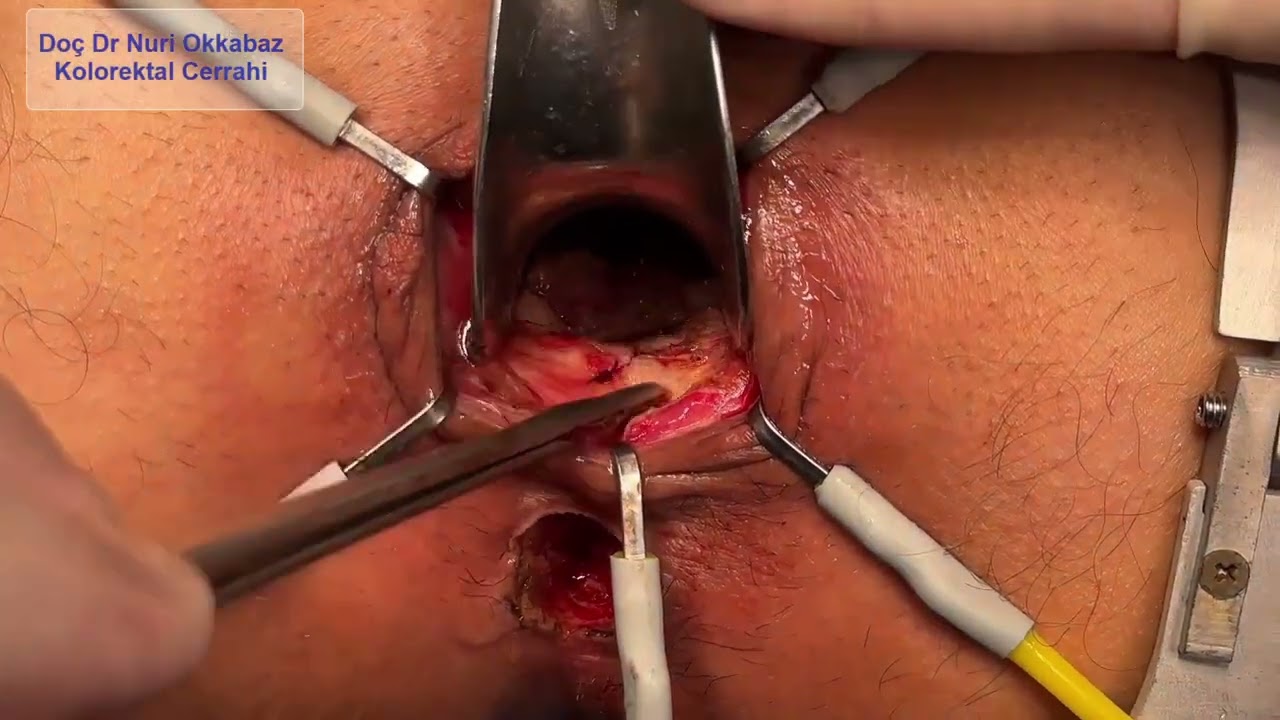
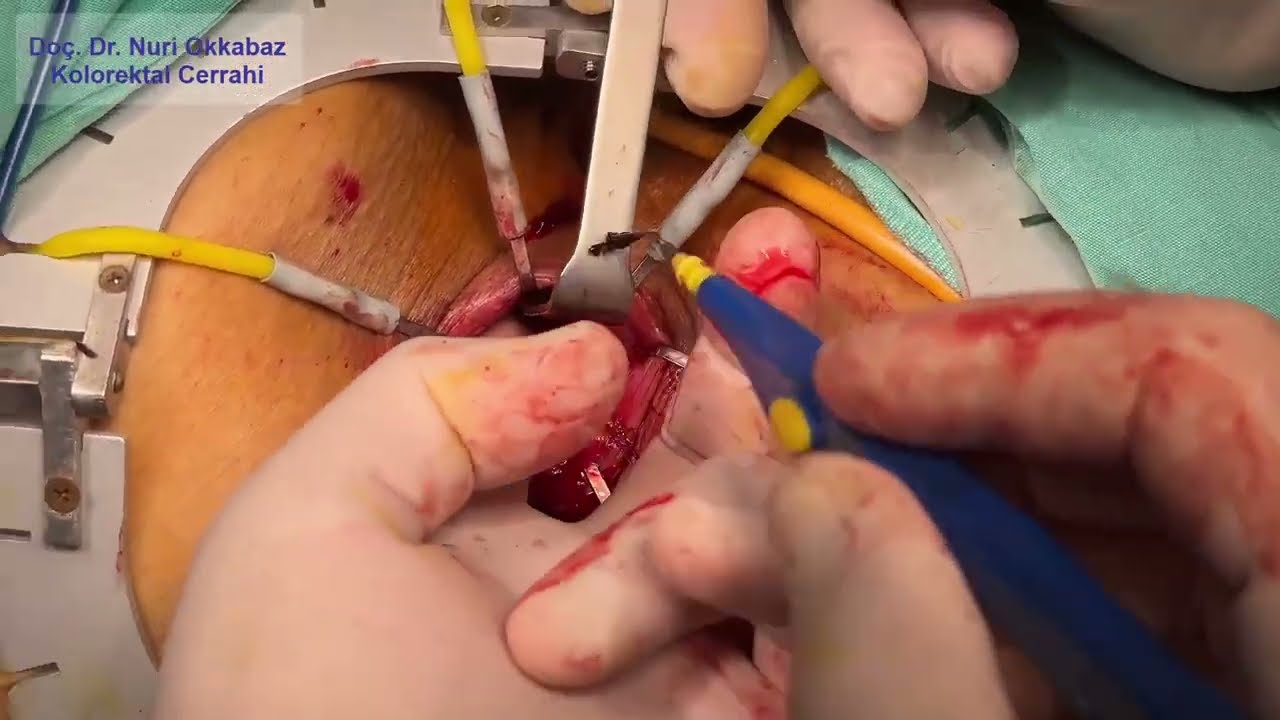
This video presents a case of fistula repair using the endorectal advancement flap technique in a patient with a recurrent anal fistula who had previously undergone surgical intervention. This method can be considered either as an alternative treatment in recurrent cases or as a first-line option for high anal fistulas.
The advancement flap technique preserves the sphincter muscles, thereby reducing the risk of fecal incontinence.
When performed by experienced hands, the endorectal advancement flap is a surgical technique with high success rates and favorable outcomes.
This video demonstrates a sphincter-preserving surgery in a patient with rectal cancer extending into the anal canal. Following laparoscopic intersphincteric dissection, the procedure continues with a perineal (transanal) approach to avoid a permanent stoma.
Although the patient had previously been advised to undergo a lifelong colostomy at another center, sphincter preservation was successfully achieved without creating a stoma. Pathological examination confirmed complete tumor resection. The patient remains under follow-up with no oncological issues observed to date.
This video shows the surgical specimen after laparoscopic resection in a patient with obstructive descending colon cancer. The patient underwent laparoscopic surgery 10 days after colonic stenting via colonoscopy. The bowel and tumor were exteriorized through a small incision, and the tumor was removed.
This approach allowed the patient to benefit from minimally invasive (laparoscopic) surgery. Instead of removing the entire colon, a limited resection with adequate oncological margins was performed. Additionally, thanks to preoperative stenting, the surgery was completed without the need for a stoma (colostomy).
This video presents the open surgical resection of a pancreatic mucinous cystic neoplasm, in which the cyst was removed intact. After separating the adhesions between the cyst, the stomach, and the transverse colon, the spleen and the pancreatic tail were dissected from the retroperitoneum. The splenic artery was ligated, and following mobilization of the pancreatic neck, the pancreas was transected. Adhesions between the cyst and the portal vein were carefully dissected, and the splenic vein was ligated, allowing complete removal of the cyst. In the final step, the remaining pancreatic tissue was sutured to prevent leakage.
Pathological examination confirmed the diagnosis of mucinous cystic neoplasm with no evidence of malignant transformation.
Various treatment methods have been described for rectal prolapse, and the most effective ones are typically abdominal approaches. However, in patients with high anesthesia risk or those who are not suitable candidates for abdominal surgery, perineal approaches can be considered. This technique allows resolution of the prolapse and improvement in defecation in high-risk patients.
In this video, we present footage of an Altemeier procedure (perineal rectosigmoidectomy) performed under spinal anesthesia in a 78-year-old patient with severe cardiac disease.
This video demonstrates the technical details of the Kono-S anastomosis performed in a patient who underwent laparoscopic ileocecal resection for Crohn’s disease.
You can watch my interview given to the media as part of the Colorectal Cancer Awareness Month activities in March here.
This includes excerpts from the laparoscopic right hemicolectomy operation in cases of cecum cancer with invasion into the abdominal wall and retroperitoneum.
This includes sections from the laparoscopic complete mesocolic excision and subtotal colectomy operation performed in cases of colon cancer located in the distal part of the transverse colon, having advanced by infiltrating the surrounding fatty tissues through the intestinal wall.
Laparoscopic colon resection performed for colon cancer located in the proximal part of the sigmoid colon, a short video.


